Table of Contents
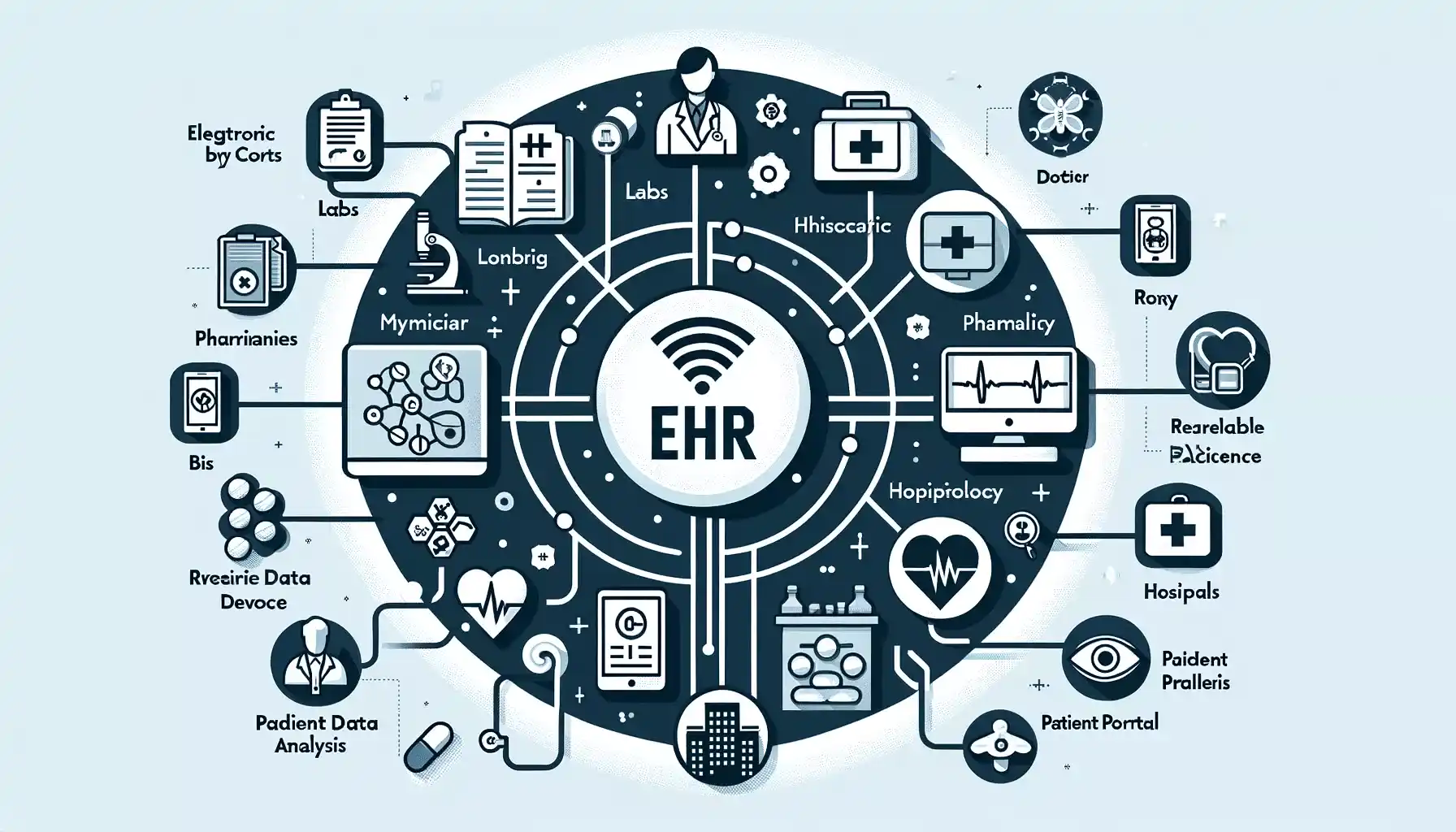
In the ever-evolving realm of healthcare, the impact of EHR systems (Electronic Health Records) stands as a pivotal force, transforming patient care and administrative processes. Beyond digitizing traditional paper records, EHRs revolutionize healthcare delivery by offering comprehensive, real-time access to patient data. This paradigm shift enables healthcare providers to deliver personalized treatment plans, streamline workflows, and enhance coordination among care teams.
In this comprehensive exploration, we delve into the multifaceted impact of EHR systems on healthcare, examining their essential functions, core components, and the challenges and opportunities they present in navigating the complexities of modern healthcare delivery.
Understanding Electronic Health Records (EHRs)
Electronic Health Records (EHRs) are digital versions of patients’ medical histories, containing comprehensive information about their health and medical care. They include patient demographics, medical history, clinical data, medication and allergy lists, and immunization records.
EHRs facilitate efficient management and sharing of health information among healthcare providers, promoting better coordination of care and improved patient outcomes. They enable healthcare professionals to access up-to-date patient information, make informed decisions, and provide personalized treatment plans.
Overall, EHRs and the impact of EHR systems play a vital role in modernizing healthcare delivery by enhancing data accuracy, accessibility, and continuity of care.
Core Components of EHR Systems
The sophistication of EHR systems lies in their multifaceted components, each serving a specific purpose in enhancing care delivery:
- Patient Demographics: Essential for proper identification and continuity of care, this section includes details like name, date of birth, and insurance information.
- Medical History: Chronic diseases, surgeries, allergies, and family medical history are meticulously recorded to provide context during treatment.
- Clinical Data: Dynamic and comprehensive, this section encompasses doctor’s notes, diagnoses, medications, and test results, facilitating informed decision-making.
- Medication and Allergy Lists: Detailed records of medications and known allergies prevent adverse reactions and ensure safe prescribing practices.
- Immunization Records: Crucial for public health initiatives, these records track immunization history for individuals and populations.

The Impact of EHR Systems on Healthcare
- Enhanced Patient Care: The impact of EHR systems grants immediate access to comprehensive data, enabling personalized treatment plans & proactive interventions.
- Improved Efficiency: Experience the transformative impact of EHR systems on healthcare. Streamlining administrative tasks and reducing paperwork, EHRs optimize workflow, freeing professionals to prioritize patient care. Seamless data exchange enhances collaboration across settings.
- Data Security: EHRs prioritize patient confidentiality and integrity with robust security measures, mitigating the risks of data breaches. The impact of EHR systems is crucial for patient privacy and regulatory compliance.
- Facilitating Research: Utilizing EHR systems, the Impact of EHR enhances research, population health management, and clinical trials. Aggregating anonymized patient data drives advancements in healthcare delivery and patient outcomes.
- Patient Engagement: Through patient portals and interactive features, EHRs empower patients to actively participate in their healthcare journey. The impact of EHR systems, providing access to personal health records, appointment scheduling tools, and educational resources, promotes patient engagement and collaboration between patients and providers, leading to improved health outcomes and satisfaction.
Essential Functions of EHRs
Beyond data storage, EHRs offer a suite of functions that revolutionize healthcare delivery:
- Data Management: EHRs compile and organize patient data, improving accessibility and productivity in healthcare settings. In addition to EHRs, EMS epcr software provides emergency services with robust tools to manage patient data in real time, ensuring critical information is accessible during emergencies.
- Clinical Decision Support: Advanced algorithms alert providers about potential issues, reducing errors and improving care quality.
- Patient Engagement: Patient portals enable interaction and shared decision-making, enhancing transparency and collaboration in care delivery.
- Interoperability: Seamless data exchange among healthcare providers ensures continuity of care and better care coordination.
- Quality Reporting: EHRs track clinical quality measures, supporting initiatives to improve healthcare outcomes.
7 proven strategies for leveraging the impact of EHR systems
- Comprehensive Data Capture: EHR systems allow for the comprehensive capture of patient data, including medical history, medications, allergies, and treatment plans. By consolidating this information in a centralized digital platform, healthcare providers gain immediate access to critical patient information, enabling more informed decision-making and streamlined care delivery.
- Standardized Clinical Documentation: Standardized clinical documentation templates within EHR systems facilitate efficient and consistent documentation of patient encounters. By adhering to predefined templates for progress notes, assessments, and treatment plans, healthcare providers can ensure thorough and accurate documentation while minimizing documentation time.
- Clinical Decision Support Tools: EHR systems are equipped with clinical decision support tools that provide real-time guidance and recommendations to healthcare providers. From drug interaction alerts to evidence-based treatment guidelines, these tools help clinicians make informed decisions at the point of care, reducing errors and improving patient safety.
- Interoperability and Data Sharing: Interoperability features enable seamless data exchange between EHR systems and other healthcare entities, such as hospitals, clinics, and pharmacies. By facilitating the sharing of patient information across different care settings, interoperability enhances care coordination, continuity, and collaboration among healthcare providers.
- Patient Engagement Portals: Patient engagement portals integrated into EHR systems empower patients to take an active role in their healthcare management. Through secure online portals, patients can access their health records, schedule appointments, request prescription refills, and communicate with their healthcare providers, leading to improved patient satisfaction and adherence to treatment plans.
- Telehealth and Remote Monitoring: EHR systems support telehealth and remote monitoring capabilities, allowing healthcare providers to deliver virtual care and monitor patients remotely. Through video consultations, secure messaging, and remote monitoring devices, EHR-enabled telehealth services extend access to care, particularly for patients in rural or underserved areas.
- Data Analytics and Population Health Management: EHR systems offer robust data analytics tools that enable healthcare organizations to analyze large datasets and identify trends in patient populations. By leveraging data analytics for population health management, healthcare providers can identify at-risk patients, implement preventive interventions, and allocate resources more effectively, ultimately improving health outcomes and reducing healthcare costs.

EHRs vs. EMRs: Understanding the Difference
| Criteria | Electronic Health Records (EHRs) | Electronic Medical Records (EMRs) |
|---|---|---|
| Definition | EHRs are comprehensive, patient-centered records that provide a full-fledged view of a patient’s health journey across different healthcare providers and care settings. | EMRs are the digital equivalents of traditional paper charts within a single practice. They offer a concise overview of a patient’s medical history, treatment plans, etc., within one particular healthcare facility. |
| Scope | EHRs compile data from all healthcare professionals engaged in a patient’s care, spanning doctors, specialists, hospitals, labs, and pharmacies. | EMRs typically include information collected within a single provider’s office or clinic. The data may include medical history, diagnoses, and treatments from that practice alone. |
| Interoperability | EHRs ensure the confidential, fluid exchange of patient data among varied health professionals. It promotes the integration of health information, improving coordination and continuity of care. | EMRs, in general, lack interoperability capabilities. They are less equipped to share data outside of the individual practice, which can potentially lead to fragmented care. |
| Role in Patient Care | EHRs serve as a valuable tool in facilitating shared decision-making and a patient-centered approach to healthcare. They can improve patient outcomes by offering a more holistic view of their health status. | EMRs serve more of a documentation role, aiding clinicians within a specific practice in tracking patient data over time, identifying patients due for preventive screenings, and managing patients with chronic conditions. |
| Impact on Healthcare Practices | The impact of EHR systems can streamline administrative tasks, expedite billing and reimbursement processes, support research and data analysis, and facilitate population health management. | EMRs primarily help clinicians diagnose and treat patients effectively within their specific practice by providing a detailed view of a patient’s medical history. They might not significantly influence larger-scale healthcare practices. |
Conclusion
In conclusion, the impact of EHR systems on healthcare is profound and far-reaching. By offering comprehensive patient records across diverse healthcare settings, facilitating data exchange among professionals, and promoting patient-centered care, EHRs revolutionize healthcare delivery. Their role in streamlining administrative tasks, enhancing research capabilities, and improving patient outcomes cannot be overstated.
While EMRs have their place in documenting patient data within specific practices, it’s clear that EHRs set a new standard for efficiency, coordination, and quality of care in the modern healthcare landscape. The adoption and integration impact of EHR systems signifies a transformative shift towards a more interconnected and patient-centric healthcare ecosystem.